High Blood Pressure (also called hypertension) is one of the most common—and most ignored—health problems today. Many people feel “normal” even when their blood pressure stays high for months or years. That’s why hypertension is often called a silent condition. Over time, it quietly damages blood vessels and forces the heart to work harder, increasing the risk of serious heart diseases like heart attack, heart failure, stroke, and rhythm disorders.
This blog explains how high blood pressure harms the heart, the warning signs, who is at risk, how it is diagnosed, and how you can control it with the right lifestyle, treatment plan & Experienced Cardiologist like Dr Gautam Naik.
Blood pressure is the force of blood pushing against the walls of your arteries. It is written as two numbers:
Hypertension is typically diagnosed when readings remain ≥140/90 mmHg on repeated measurements.
Some guidelines classify lower ranges (like 130–139/80–89) as stage 1 hypertension and recommend treatment based on overall risk.
Key takeaway: Even “mildly high” BP can harm the heart if it remains uncontrolled for years.
Your heart is a muscle that pumps blood through arteries to the whole body. When blood pressure stays high:
This damage is gradual, so people often discover hypertension only after complications occur.
High pressure injures the inner lining of arteries. Over time, arteries can become less flexible and narrower. This makes it harder for blood to flow smoothly, and it contributes to plaque buildup (atherosclerosis). Narrow arteries reduce oxygen supply to the heart muscle—setting the stage for chest pain (angina) and heart attack.
When the heart constantly pumps against high pressure, the left pumping chamber works overtime and may thicken. This is called Left Ventricular Hypertrophy (LVH). A thickened heart muscle can become stiff, and pumping becomes less effective. Over time, this increases the risk of heart failure, rhythm issues, and complications.
High BP adds continuous workload on the heart. Initially, the heart may enlarge or thicken to cope, but eventually it may weaken or stiffen, leading to heart failure—a condition where the heart cannot pump enough blood to meet the body’s needs.
High blood pressure accelerates artery damage and plaque formation. If a plaque ruptures and blocks blood flow to the heart muscle, it can cause a heart attack. This is one of the biggest long-term dangers of uncontrolled hypertension.
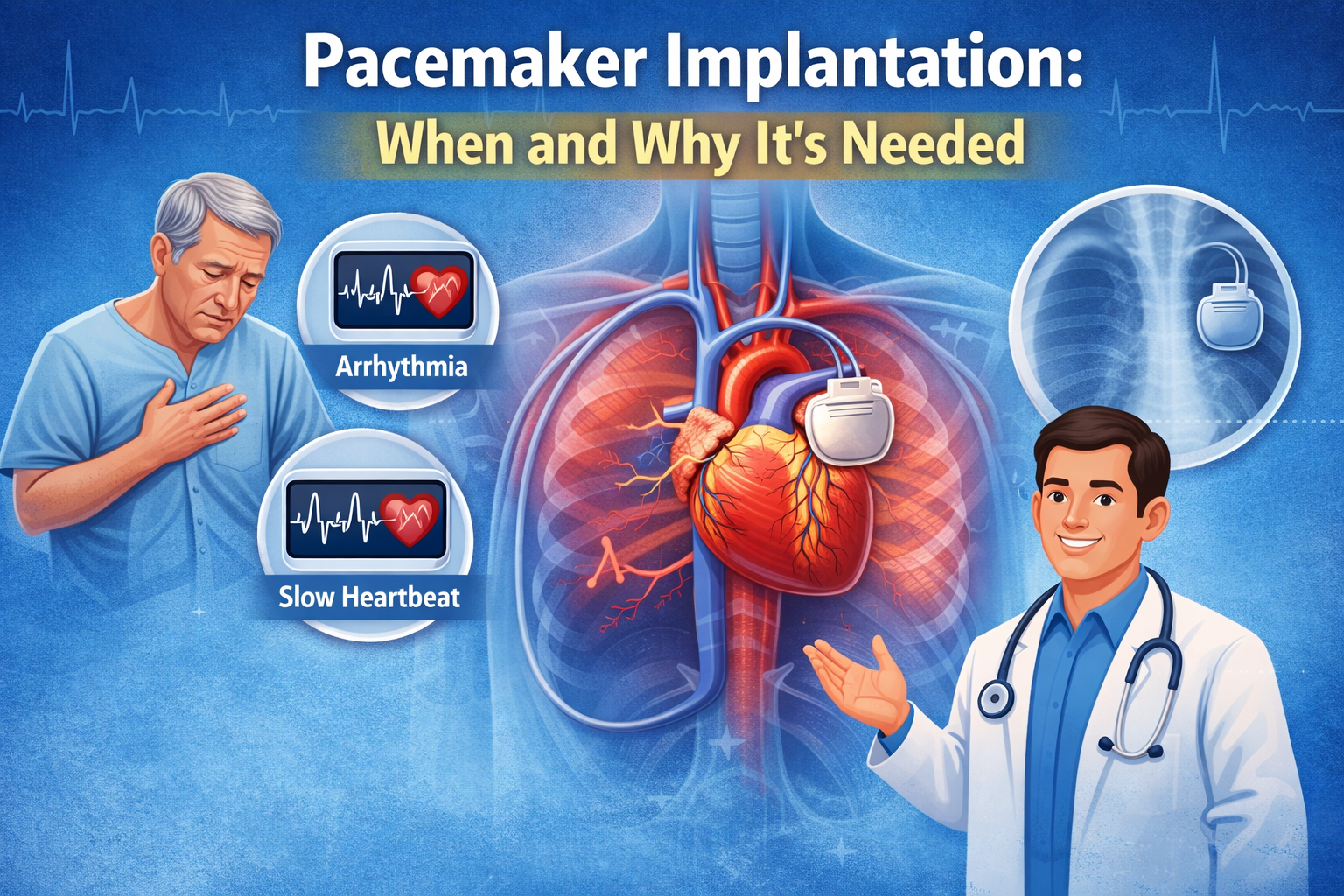
Changes in heart muscle structure (like LVH), stress on the heart, and reduced oxygen can increase the risk of irregular heartbeats. Some arrhythmias—such as atrial fibrillation—also increase stroke risk and need proper management.
Long-standing hypertension may contribute to strain on heart valves and worsen existing valve problems. When the heart enlarges or stiffens, valve function can also be affected.
Most people don’t feel anything for a long time. That’s why routine checks matter.
However, when blood pressure becomes very high—or when complications begin—some people may notice:
Important: These symptoms are not specific, and many people have no symptoms at all. Don’t wait for signs—measure regularly.
You are more likely to develop high blood pressure if you have:
Many people have multiple risk factors together, and that is when heart risk increases significantly.
Correct measurement matters because BP can appear high due to stress, caffeine, or wrong technique.
Better practice includes:
Modern guidelines also encourage home BP monitoring and, when possible, out-of-office measurements to get a more accurate picture.
If you have high blood pressure—especially long-standing or uncontrolled—your cardiologist may advise tests to check heart impact and overall risk, such as:
The goal is not just to “reduce numbers” but to prevent damage to heart, brain, kidneys, and eyes.
Targets differ based on age and medical condition. Many clinical recommendations aim for tighter control in suitable patients, and some guidelines suggest targets like <130/80 for many adults when tolerated, especially in those at higher cardiovascular risk.
But here’s the practical truth:
Your ideal target should be personalised by your cardiologist based on:
Even if medicines are needed, lifestyle changes improve results and reduce long-term risk.
Indian diets often include hidden salt from pickles, papad, namkeen, sauces, packaged snacks, and restaurant food. Reducing salt can meaningfully reduce BP in many people.
Even modest weight loss can lower BP and reduce strain on the heart.
Aim for at least 150 minutes/week of moderate activity (like brisk walking), as advised by your doctor—especially if you have heart symptoms.
Tobacco damages arteries and multiplies heart attack risk when combined with hypertension.
Alcohol can raise BP and affect rhythm.
Chronic stress and poor sleep increase BP and worsen heart health. Addressing sleep apnoea (if present) is especially important.
Focus on:
Many people worry about “starting BP medicines for life.” But if your BP is consistently high, medicines can protect your heart, brain, and kidneys. Treatment is decided based on BP level and overall cardiovascular risk.
Common categories include:
Important:
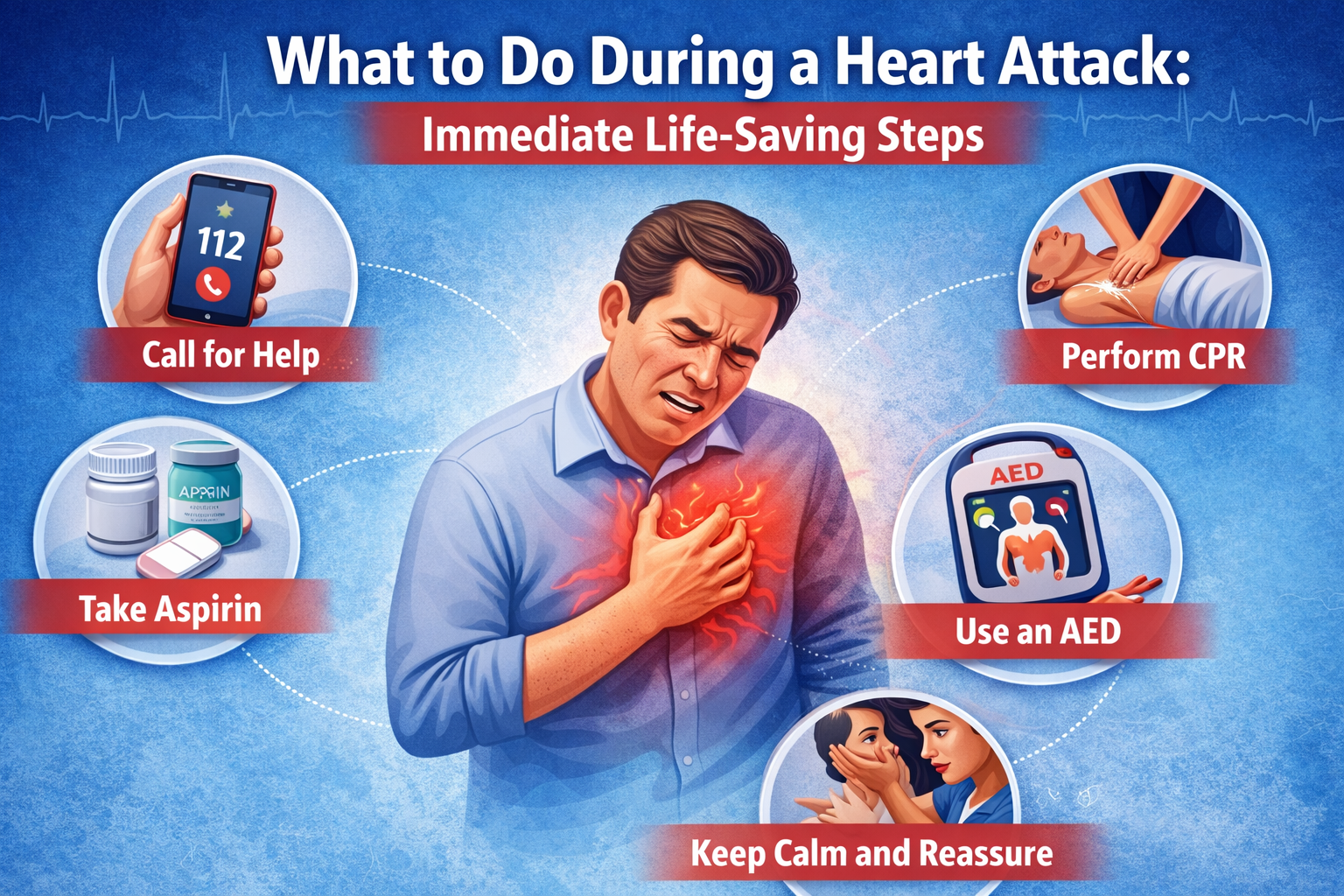
Go to emergency care immediately if BP is very high with symptoms like:
These can signal heart attack, stroke, or hypertensive crisis and must be treated urgently.
A cardiologist does more than prescribe a BP tablet. The right specialist:
If you want expert cardiac guidance for hypertension and heart risk, Dr Gautam Naik is widely regarded as the best Cardiologist in Delhi at Apollo Hospital, known for patient-focused evaluation and evidence-based treatment planning.
Yes. It damages artery walls and accelerates plaque buildup, increasing the risk of blockage and heart attack over time.
Yes, this can happen (often called “white coat effect”). That’s why home monitoring and proper technique are important.
Most BP medicines actually protect the kidneys, especially in diabetes or chronic kidney disease. Your doctor will choose what suits you.
Often yes. Hypertension can damage the heart silently.
Some people improve within weeks; others need a few months of adjustment. Consistency with lifestyle and medicines is key.
High blood pressure is not just a “number problem.” It is a heart health problem. The earlier you detect it and control it, the more you protect yourself from heart attack, heart failure, and long-term damage.
If you want a second opinion or a comprehensive heart risk assessment, consider consulting Dr Gautam Naik, the best Cardiologist in Delhi at Apollo Hospital, for personalised guidance on hypertension control and heart protection.